"It feels like you are back in the womb," Melinda says. "It melts everything away. All you feel is bliss."
Melinda, now in her 40s, was introduced to heroin by a boyfriend in college. Right away, she loved it. It felt good. Heroin also fit into the story she and her friends had created for themselves. "We idolized artists and writers who experimented with psychedelics and journeying outside the norm," she says. "I had a rough childhood. Heroin made it feel like all of my problems disappeared."
Her problems may have disappeared temporarily, but they came roaring back when the drug wore off. This only made her want it more. "I thought heroin was so romantic," she says, "but it wound up making my life smaller and smaller and smaller."
When she was in her 20s, living in DC and working as an editor at a magazine, Melinda's life started to fall apart. She would be in meetings and all she could think about was going home and getting high. She watched friends overdose, commit suicide, and go to prison. Still, she kept using. She had intense mood swings and difficult relationships. And she was getting increasingly sick. One day at work, she went into the bathroom and threw up. "It was obvious I couldn't function at that point," she says. By the end of the day, she'd quit her job.
Melinda knew she needed to get away from her old life, so, soon after, she packed up and moved to the West Coast. She floundered for a while, trying to make work connections and get clean on her own, before ending up in a rehab facility in Los Angeles. She was hopeful about recovery there, but during her stay, she says, a counselor raped her. She left rehab more traumatized than when she went in.
This was just the beginning. Over the next two decades, Melinda would try many different ways to get clean. And after multiple relapses, including a nine-year struggle with opioids after she was prescribed Vicodin and Percocet following surgery, she did, eventually, get clean. But it wasn't rehab that saved her, and it wasn't 12-step programs or even abstinence that did it. The thing that saved Melinda was smoking weed.
Between 1999 and 2016, the number of opioid deaths in the United States quadrupled, and the Centers for Disease Control and Prevention says that today about 91 Americans die every day from overdosing. The vast majority of these drug deaths occur when users—either inadvertently or by choice—mix opioids with other substances, including alcohol, benzodiazepines like Xanax, or even over the counter painkillers like Tylenol.
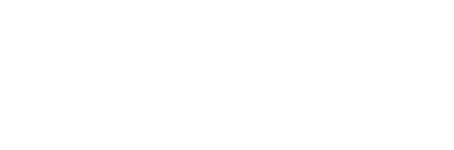
While drug deaths are hardly new, what is new is who is dying, says Shilo Jama, executive director of the People's Harm Reduction Alliance, an advocacy group for drug users in Seattle. "The only reason anyone gives a shit is because middle-class white people are dying," Jama says. "People have been dying in the city for decades, but no one cared until middle-aged soccer moms started calling their legislators demanding a fix to this 'crisis.'"
Still, statistics show us that drug deaths are up. And beyond death—and the destruction of families and communities—there are also the financial impacts of addiction on society. The National Institute on Drug Abuse estimates that prescription opioid abuse alone—not including heroin—has cost the United States more than $78.5 billion, including in health care, criminal justice, and loss of productivity.
Part of the reason opioids are so deadly, and so costly, is because once you are on them, it can be almost impossible to stop. Opioids and opiates—which include heroin as well as synthetic drugs like Fentanyl, OxyContin, Percocet, Vicodin, and Demerol—cause a flood of endorphins in the brain. This produces the blissed out, womb-like feelings Melinda experienced in the beginning of her heroin use. But over time, the brain stops producing these feel-good chemicals on its own. Users start to feel sick, depressed, and anxious, and instead of taking the drugs to get those warm feelings, they start taking them to stave off withdrawal. At that point, there's no pleasure left.
"It feels like your body is breaking down and fighting against you," Melinda says. "There is something inside of you that makes you want to get more and more of it even though you know it's ruining your life and taking away all the joy and the hope and the love. You see all that happening but you can't stop."
For many addicts trying to get off drugs, methadone helps. Often called the "gold standard" of opioid treatment, the California Society of Addiction Medicine estimates that success rates for methadone patients range from 60 to 90 percent. Twelve-step programs like Alcoholics Anonymous and Narcotics Anonymous, by comparison, have an estimated success rate of only 5 to 10 percent, while success rates for both in-patient and out-patient rehab programs—which can cost anywhere from $1,000 to $90,000 a month—are rarely made public. (The rehab industry is unregulated and programs can, and do, claim whatever success rates they want, according to Lance Dodes, psychiatrist and author of The Sober Truth: Debunking the Bad Science Behind 12-Step Programs and the Rehab Industry.)
Still, while studies show that methadone—which works by relieving opioid cravings while blocking euphoric effects—is the most effective treatment for opioids, it can be fatal, and it's difficult to get. Methadone providers are strictly regulated by both state and federal laws, which requires that patients show up in person to get their doses, even if the clinic is miles or hours away. In King County, there are about a dozen clinics and three providers, and there are strict limits on how many patients they can serve. Evergreen Treatment Services, a nonprofit methadone provider with locations in Seattle and Renton, has a maximum capacity of 2,000 patients. That's not enough to serve the county's needs, according to clinic manager Sean Soth.
For those who can't get into Evergreen or other nonprofit programs, there are private, for-profit providers as well. One of those, Kent Treatment Solutions, is owned by multinational corporation Acadia Healthcare, which operates 576 "behavioral health-care facilities" in 39 states. For patients without health insurance, methadone there costs $220 to enroll and $430 a month—more if you get it by the week.
In you can find treatment, there are other hoops to jump through, like working with a case manager, attending support groups, and submitting to drug testing. In the past, according to Shilo Jama, people have been kicked out of programs for such minor offenses as showing up in their pajamas, which is perceived as "drug-using-like behavior."
Although methadone has proved to be the most effective form of opioid treatment, it just wasn't available for Melinda—or for most Americans: Studies have shown that between 80 and 90 percent of opioid addicts are unable to access the treatment they need. Weed, however, Melinda could get, so she gradually tapered her drug use under doctor supervision and used cannabis to help with the symptoms of withdrawal. She says the weed would pause the discomfort long enough to get through it. She did this twice to get off heroin, and later she did it to get off the opioids she'd been prescribed after brain surgery.
But cannabis substitution doesn't work for everyone. "Marijuana may alleviate some symptoms, but you are still going to go through a pretty intense withdrawal," Jama says. Plus, it's a vastly different high, one that might not be appealing to all users. "But if marijuana substitution makes you a more stable drug user, we are fully supportive of that," he says. "We want people to have productive lives."
Regardless of how helpful weed may be, it isn't magic. It won't change the places you go or the people you see. For some opioid users, 12-step programs can be helpful as well, offering fellowship, structure, and support when the itch starts up. But these groups aren't always amenable to drug substitution. While a spokesperson for Narcotics Anonymous told me that meetings are open to all users, their official stance is "abstinence, not replacement."
Melinda and her partner, who is also in recovery, did attend NA for a time, but they got stuck on the fourth step: taking a "searching and fearless moral inventory." As part of this step, they felt it important to tell their sponsors that they were using medical marijuana. They were, Melinda says, "stonewalled."
There have been few scientific studies on cannabis as a substitute for opioids. That's by design. Because cannabis is still labeled a Schedule 1 drug—meaning, according to the federal government it has no medical value and a "high potential for abuse"—it is exceedingly difficult to get permission to study the plant's effects, requiring approval from both the Drug Enforcement Administration and the Food and Drug Administration. And even in places with pot shops down the street, all research weed must come from one government-approved cannabis lab at the University of Mississippi—which has been accused of supplying low-potency and contaminated samples.
There are, however, work-arounds. Instead of randomized, controlled trials where researchers give opioid users either cannabis or a placebo and then measure the outcome, researchers can study opioid users who voluntarily enroll in medical marijuana programs.
One of these studies' results were published in September in the Journal of the American Medical Directors Association. "We compared two groups of patients with a chronic pain diagnosis," says study author Jacob Miguel Vigil from the University of New Mexico. One group chose to enroll in New Mexico's medical cannabis program and the other chose not to. Over five years, researchers compared the two groups' prescription activity. What they found is that the group enrolled in the cannabis program showed significant reductions in both opioid use and other prescription drugs like benzodiazepines, used to treat anxiety. "It basically suggests that cannabis may be more effective in not only treating patients on certain classes of prescription drugs like opiates, but perhaps a broader spectrum of controlled medications," Vigil says.
Vigil thinks cannabis has the potential to help with heroin withdrawal as well. "People coming off heroin are managing to bridge their withdrawals through cannabis," he continues. "I hear it all the time. All the time." And, as Vigil points out, cannabis is a lot safer than some government-approved treatments: Methadone overdoses killed 3,400 people in 2014. Cannabis didn't kill any.
Of course, it's not as simple as just putting down the needle and picking up the pipe.
Even for Melinda, who readily attributes cannabis to her recovery, it took much more than just smoking weed to get clean. She changed the people, places, and things that she felt were holding her back. She developed new habits, found new friends, and made recovery a central tenet of her life. Melinda has some unconventional attitudes toward medicine—she credits cannabis with curing her Lyme disease and she practices both energy healing and sound bathing—but it works for her. She's active in both online and offline communities for marijuana maintenance, as cannabis substitution is often called, and she works as a trauma counselor, where, she says, she recommends weed to her clients almost daily.
There's no one right path toward recovery, but Melinda finally found her way out of addiction, 24 years after she first got high. It wasn't what most health-care providers or drug counselors would recommend, but she isn't alone: Whether America is ready for cannabis substitution or not, it's happening, all across the country, as people tackle the opioid crisis on their own. Melinda knows she'll never have that blissful, womb-like feeling again, but she's okay with that now. She's got cannabis—and with it, her life back.