It was a promising idea. Our infection-fighting immune system hates cold viruses. If we put HIV proteins into a cold virus and inject the engineered mix as a vaccine, the immune system should fight off HIV like it does a cold. A vaccine like this may not stop someone from becoming infected with HIV, but it might at least stop or delay the progression to AIDS.
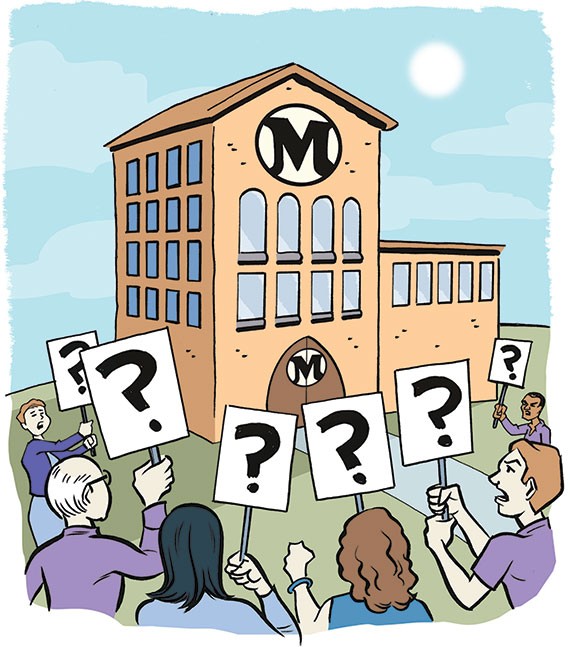
After some successful experiments in primates, a massive HIV vaccine trial—the STEP trial sponsored by Merck—was started in 2004 with 3,000 volunteers worldwide, including 119 gay men in Seattle. The trial, like several others, was based out of the HIV vaccine trials unit in Seattle at the Fred Hutchinson Cancer Research Center. "This was the first vaccine to get this far in quite a while," noted Hunter Kincaid, one of the Seattle volunteers.
In a scheduled peek at the raw data earlier this fall, it became obvious that the vaccine couldn't protect anyone from getting HIV (as expected) nor reduce viral loads in those infected—a surprise big enough to halt the vaccine injections. A deeper look at the data revealed something much worse. People who had been infected with a version of this cold virus before starting the trial seemed to have a higher risk of getting HIV than those who had not been vaccinated—a shock to everyone involved.
Now, after the trial has been abruptly stopped, Kincaid sounds more skeptical. "I propose a new rule in science," he says. "If you want to test a new vaccine, you have to inject it into yourself as well; maybe then they will do more preliminary research."
Meanwhile, nearly 800 people involved in the vaccine trials are now more vulnerable to HIV infection. On November 13, the leaders of the study decided to tell volunteers if they received the vaccine and are more susceptible to acquiring the HIV virus, or if they received the placebo. Kincaid is still waiting for test results to see which group he is in.
The news that the vaccine may have backfired was reported in a November 8 New York Times article "In Tests, AIDS Vaccine Seemed to Increase Risk." The article described the results as a ''puzzling and potentially troubling development" in a test of "one of the most promising experimental AIDS vaccines to have been tested on people." Dr. Larry Corey, one of the scientific leaders of the trial, was quoted as saying: "We did a beautiful experiment, but it definitely was a disappointment."
Kincaid sounds bitter about that assessment: "Personally, I think calling it a beautiful study is a bit insensitive to those of us who volunteered our time for their 'beautiful study' and were instead put at increased risk of HIV infection."
Kincaid, now a graduate student in Chicago, but at the time an employee at Fred Hutchinson Cancer Research Center, joined the trial in 2005 because "volunteering to help out in the creation of an HIV vaccine was a big deal. You volunteer your efforts where you can, and they were having trouble recruiting enough people." Kincaid, only in his early 20s, came out after drug therapy could combat HIV. He says that HIV "is less of a lived fear for my generation."
Another volunteer, W. F.—a physician in his mid-40s who was in the placebo test group—is from a generation with a different perspective on HIV. W. F. can acutely recount what HIV infection was like before effective drugs became available. "My partner was down to around 50 T-cells before the protease inhibitors came out—they saved his life." So, W. F.'s reasons for volunteering were both intimate and rational. "I considered it my duty to participate, both as someone with a personal interest in the disease and a professional obligation to help people. The premise of the vaccine was interesting to me and I thought it held promise."
W. F.'s reaction to the failure is mixed, though. He believes the screwup has implications for the next large-scale anti-HIV vaccine trial. "The fact that this vaccine may increase vulnerability to HIV infection will scare away thousands of potential volunteers from any new study. Worse, it'll make it very hard to get any vaccine study approved by a review board at any academic hospital, at least until the mechanism of this failure is fully understood. That will take years."
W. F. is guardedly hopeful that enough people will volunteer for the next, much smaller pilot trials. "It will ultimately take a few hundred people who have a loved one who's been hurt or killed by the virus to step up and, yes, take a chance with their lives. They will be a little harder to find next time around, but I still think they're out there." Even with the shockingly bad results, he remains happy he participated in this trial: "I considered it a privilege to be included in this study, and I'd sign up for another one in a second if they'd have me."
Dr. Karen Mark, clinic director for the Seattle site, stands by the trials. ''No one wants to hear this experimental HIV vaccine may have increased people's risk of infection,'' she acknowledges. ''But the people I've spoken with in the community realize the importance of developing an HIV vaccine. The study worked the way it was supposed to, getting the answer as quickly as possible. We're not closing up shop here." Dr. Mark points out the failed STEP trial continues to be of use. The blood samples collected along the way can help unravel what exactly went wrong with this vaccine. If nothing else, all local participants in this study received extensive counseling on how to avoid HIV infection.
Hunter is still waiting to find out if he received the vaccine, and if his blood had evidence for a prior infection with this cold virus. He has a call in, but the answer hasn't yet arrived. ![]()