In 2018 742 people died from opioid overdoses in Washington state, and about half of those cases involved prescription opioids.
A proposal working its way through Olympia seeks to decrease those numbers with a simple solution: Every time a doctor prescribes a risky amount of opioids, that doctor must also prescribe the antidote—naloxone—or confirm the patient already has a prescription for it.
A bunch of empirical data shows that increasing "overdose education and naloxone distribution" reduces overdose deaths and increases "quality-adjusted life years." Though this bill would do just that, first responders and nurses are having an intense but respectful debate with doctors groups over the issue of mandating access to this life-saving drug.
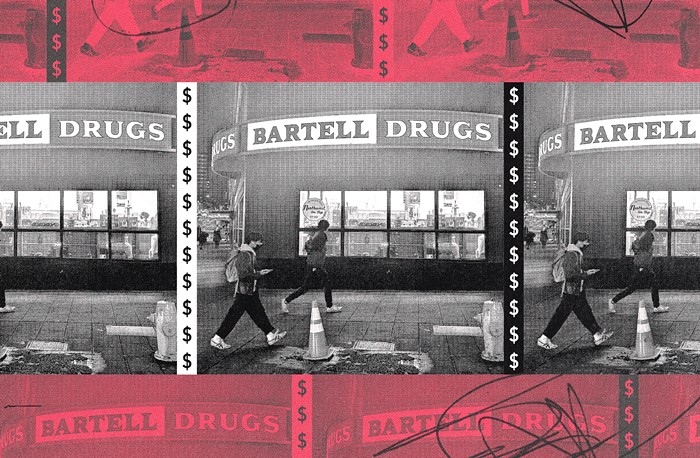
A.J. Johnson, a Snohomish firefighter who works for the state firefighter's lobby, said he's been on hundreds of OD calls in the last few years. Despite the public perception of the opioid crisis as a street problem, Johnson says "a lot" of people are accidentally overdosing or abusing opioids in their homes. Johnson's experience is backed up by recent reports from the Centers for Disease Control, which show that, over the last few years, "most overdose deaths occurred in homes."
Johnson supports the bill as "a step in the right direction" that would help save lives and reduce medical costs. "If we can get the antidote on board while the fire department is en route to their house, we can avoid any long-term problems or hospital stays," he said.
Sen. Marko Liias, who sponsored the bill, said during testimony last month that such a mandate would also create space for a "teachable moment" in doctor's offices, ensuring that doctors are telling their patients about the risks of opioid addiction and overdose as they're prescribing the drugs.
A slate of lobbyists representing various doctors groups, however, oppose the bill largely on the grounds of autonomy. They note that in 2017 the legislature created five prescribing boards responsible for setting these kinds of co-prescription rules for different prescribing groups (e.g. dentists, podiatrists, bone doctors). Since these rules already exist, Katie Kolan of the Washington State Medical Association argued during testimony, there's no reason for the state to intervene and mandate this standard of care.
Moreover, Kolan argued, doctors are already supposed to talk about potential dangers and side effects of drugs they prescribe, so these "teachable moments" Sen. Liias and others are looking for are already happening.
Another lobbyist suggested that a prescription for naloxone on a medical record might make it more difficult to obtain life insurance. Two life insurance companies did deny a policy to one Massachusetts nurse a couple of years ago, but that pissed off a lot of health care professionals, who are working to make sure that doesn't happen again. Meanwhile, a spokesperson for Washington's Insurance Commissioner said life insurance companies can't deny polices based on a naloxone prescription in this state.
Though it's true these co-prescription rules already exist, they're not consistent across the board(s). In alignment with CDC's guidelines, the nurse practitioners board, for example, already uses the bill's opioid dose threshold. That is, if a nurse practitioner prescribes a dose of 50 mme per day, they also prescribe naloxone. And they do that for good reason. The CDC found that dosages at or above 50 mme per day double the risk of overdose compared to dosages below 20 mme per day. But physicians and dentists only co-prescribe naloxone with opioids for patients they deem "high-risk," and osteopaths and podiatrists only co-prescribe in more complicated circumstances.
And though the boards have these rules in place, a 2019 analysis from the CDC shows that doctors aren't prescribing naloxone to enough patients taking high doses of opioids. "Only one in 69 patients receiving high-dose opioids gets a naloxone prescription," the study found. The same study also found, perhaps unsurprisingly, that a majority of the patients not getting these potentially life-saving scripts are Medicaid patients. According to another CDC study, 45% of people who died from prescription opioid overdoses in Washington state were Medicaid enrollees. So, in Washington at least, Medicaid enrollees are disproportionately impacted by prescription opioid overdose death, but they have the lowest rate of naloxone scripts issued.
During testimony on the bill, Brad Finegood, a strategic advisor at Seattle/King County Public Health, underlined this point. "Last year out of 10,219 Medicaid beneficiaries with an opioid disorder, only 38 had a prescription filled," he said.
We're simply not getting the antidote into the hands of the people who need it the most. While it does seem a little rude for the state to force doctors to prescribe anything, and while a prescription for naloxone probably wouldn't help a person who lives alone, a universal bill like this one will dramatically increase access to a life-saving drug, and, if nothing else, make more doctors have a conversation with patients they don't appear to be having every time they write a big script for opioids.