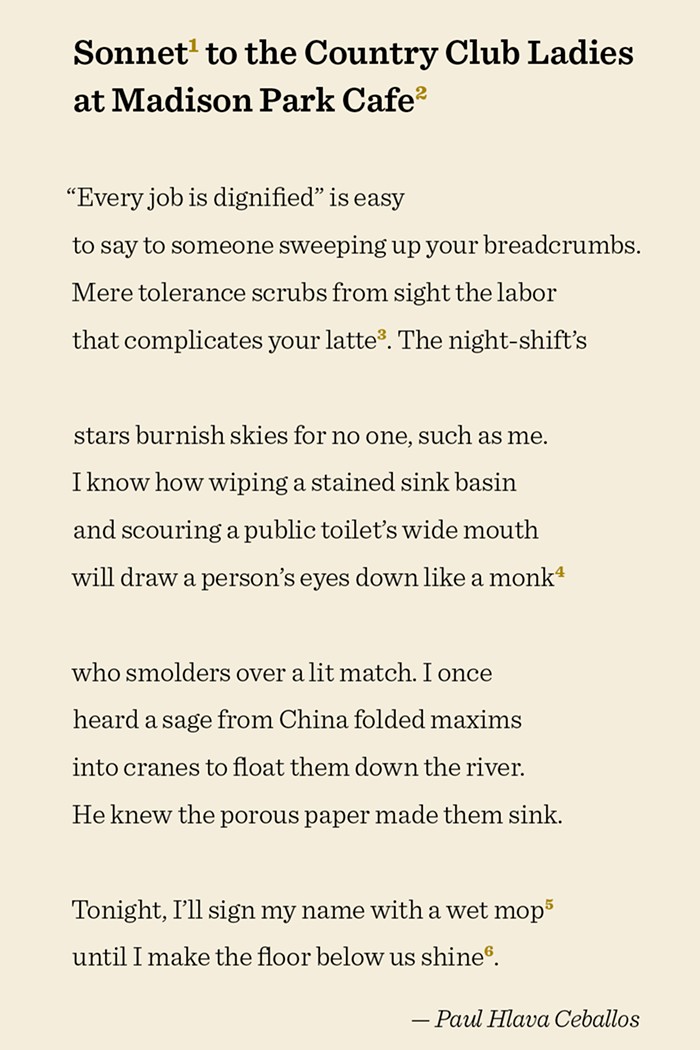
- Everett Historical/Shutterstock
- Syphilis used to be hard to treat, as this engraving depicting a 16th-century syphilis patient in Europe—and his treatment with a potion made from tree wood!—shows. It's not so hard to treat today, but it definitely can't be treated if you don't know you have it.
There's been a bit of an ocular syphilis outbreak locally—four cases in King County in December, and two more statewide, with all four of the King County cases identified among gay men. (We don't have gender or sexuality information for the two cases outside of King County, but it's worth noting that the usual rate of ocular syphilis cases for the entire state of Washington is around one a month.) If untreated, a syphilis infection can attack the nervous system and cause permanent blindness, as it did with two of the recent patients in King County.
You really do not want to get ocular syphilis. But if you do get it, Seattle's one of the better cities to be in terms of figuring out the strain that struck you. We're one of the only places in the country that can do a molecular DNA test, invented by Dr. Sheila A. Lukehart at the University of Washington, to identify syphilis strains. Previously, the only way to examine syphilis was to study it in rabbits, which tends not to happen during human outbreaks since most STI clinics don't keep an abundant supply of rabbits on hand.
Public Health is understandably eager to get this local flare-up under control—no more cases of sudden permanent blindness, please. The agency has had additional reports since the initial six cases were first discovered, but so far nothing's confirmed beyond those six, so the extent of the outbreak is still vague.
Tests are under way now at UW, and we should know more about this particular strain in a couple of days. "There appear to be types that are more likely to cause brain infections," said Dr. Matthew Golden, director of public health in the King County HIV/STD Program.
But in the meantime, here's what you need to know to keep yourself in the uninfected column:
Obviously, get tested. Go at least once a year, or every three months if you're at elevated risk. Doing poppers or meth, having had a recent STI, not knowing your status, or having had 10 or more recent sex partners all mean that you're at risk. Having had 10 or more recent sex partners also means that you can probably cool it until after Fleet Week, Blanche.
Of the four recent King County cases, all four were men who have sex with men. Three of them were HIV-positive, though only one was getting any HIV treatment. One of the patients refused treatment at first, but eventually a team of medical providers was able to change his mind. Treatment for syphilis is usually just one shot, but you don't have much time to get it before permanent damage can set in—sometimes as little as a few weeks.
There may have been more ocular syphilis cases than just these six, since cases could have gone undetected if nobody thought to correlate a patient's vision problems with an STI. Make sure you report any visual problems when you get tested.
Primary symptoms of ocular syphilis: blurry vision, floating spots, a blue visual tinge, flashing lights, or eye pain. Syphilis also causes sores, a rash, and eventually organ damage. You can also show no symptoms at all, so again, get tested. (Or, you know, lose your liver, it's up to you.)
Nobody's quite sure exactly why this outbreak is happening, but one factor might be that some HIV-prevention techniques don't protect against other infections. That includes serosorting (choosing partners based on HIV status) and then forgoing a condom, or using PrEP, a treatment that virtually eliminates the risk of HIV acquisition when taken correctly.
"I think many of those behaviors may help people decrease the risk of HIV," said Dr. Golden. "But they don't affect your risk of getting syphilis. Or may increase the risk of getting syphilis."
"That's an issue that we're dealing with here," said Gay City Health Project Wellness Center director Amber Tejada. "The assumption that there are more syphilis cases because people are having more condomless sex. Speaking anecdotally, we saw around three thousand folks for screenings in 2014, and there was not a significant increase in people reporting that they were having condomless sex." She added, "I wouldn't associate PrEP with this new outbreak."
Public Health is doing a study right now to determine the effect of PrEP on condom usage. It's scheduled to end this year, though Dr. Golden says that "if we can, we'll keep it going."
Still, PrEP remains one of your best bets against HIV, and condoms against many other STIs. For the foreseeable future, you'll want to employ a variety of techniques, including condoms, testing, and disclosing your status.
But please do not keep a hutch of bunnies in your backyard as a sort of artisanal bespoke STI testing laboratory. This is Seattle. We do polymerase chain reaction testing here.