When the American College of Emergency Physicians graded every state back in 2014, it gave Washington a D+. Among our state’s worst marks: psychiatric beds. Washington has just 8.3 beds for every 100,000 people, worse than all but two other states.
Lawmakers have wrung their hands about this shortage—and the resulting traumatic “boarding” of mental health patients—for years. Now, the University of Washington is poised to make the shortage worse.
Facing a financial crunch, UW Medicine is considering closing part or all of the psychiatric unit at the University of Washington Medical Center (UWMC), a spokesperson confirmed. The unit is currently licensed to operate 20 beds, but only operates 10 after recent staffing decreases. It admits about 430 patients per year, according to UW Medicine, and 26 nurses, doctors, and other staff work in the unit.
If the unit closes, psychiatric patients will be left to seek care from other hospitals in the region, and nurses and doctors will be laid off. The potential closure has left many in the psychiatry unit anxious. Health care providers worry about the fate of their patients in a state with a severe shortage of beds for people needing inpatient psychiatric care.
“We’re worried, we’re depressed,” said Anita Stull, a psychiatric nurse who has worked in the UW Medical Center psychiatric unit for 18 years. Stull works the night shift and says she often takes calls from people all over the state looking for help.
Media coverage and lawsuits in recent years have highlighted Washington’s dismal ranking for psychiatric beds. A 2013 lawsuit challenged the practice known as boarding, in which patients are held in emergency rooms that are not certified for psychiatric treatment—sometimes strapped down to beds in hallways—due to the bed shortage. The Washington State Supreme Court ruled that boarding is illegal. The state has since made policy changes and opened new beds, though some say it’s still not enough.
Two other nurses in the UWMC unit described their fears about the potential closure. “There will be more suicides and more bad outcomes,” said one nurse, who spoke on the condition of anonymity for fear of retaliation. “Emergency rooms will be even more overflowing. Patients won’t get the care that they deserve.”
Tina Mankowski, a spokesperson for UW Medicine, confirmed the potential closure of the UWMC psychiatric unit, which she said is due to the unit’s financial losses and expensive upgrades that would be necessary to keep it open. UW Medicine might expand psychiatric beds at Northwest Hospital in North Seattle in 2019, Mankowski said. Northwest’s psychiatric unit currently provides psychiatry for seniors.
If the UWMC unit closes, it's unclear exactly when that would happen. Mankowski said no final decisions have been made.
If UW indeed opens new beds at Northwest, the shortage could be mitigated. Still, nurses worry the Northwest unit provides a different kind of care and there could be a gap between their unit’s closure and the potential opening of new beds at Northwest.
“These are your family members and your friends,” Stull said. “People need to have some place to go.”
Nurses say the UWMC psychiatric unit, sometimes called “Seven North,” is unique among psychiatric units in western Washington. It's a primarily voluntary unit. While involuntary units treat people who are believed to be a danger to themselves or others and are involuntarily committed, people willingly check in to voluntary units. Instead of patients who are experiencing severe psychosis, patients in voluntary units are sometimes experiencing their first-ever psychotic break or suicidal ideations, the nurses said. That makes Seven North a place that's more accessible for timid patients who need help, including UW students and young mothers experiencing postpartum, they said.
One former patient who lives in Helena, Montana, described being too afraid to seek care from a state hospital. Experiencing insomnia and Xanax addiction, she flew to Seattle to check in to the UWMC unit. “It just seemed like a really safe place,” she said.
The unit treats people with “high-risk pregnancies,” meaning they are experiencing psychosis or substance abuse while pregnant. It’s also a teaching hospital, where medical students learn on the job.
“The mental health crisis, people who are chronically mentally ill...should be front and center in many ways, but we can’t forget about all the people who just periodically suffer from mental illness and are generally functioning in this world,” said another nurse who spoke on the condition of anonymity. “There are not very many places at this point for those people.”
Psychiatric care is not a money-maker for hospitals. Last year, UW Medicine had a $75 million operating loss across its multiple hospitals and clinics. Of those hospitals and clinics, UW Medical Center, which includes the psychiatric unit, had the most dramatic shortfall in 2016 and 2017, according to a presentation from UW Medicine to the UW Board of Regents. Nurses describe vacant positions left unfilled in the unit, which they believe has been “left to atrophy.”
Worsening the financial issues, the unit and other psychiatric hospitals now face costly required upgrades. Known as "ligature risk policy," federal regulators are requiring psychiatric hospitals and units to update their facilities to reduce the risk of hanging or strangulation. This includes not just removing cords and ropes but also doors, hooks, windows, and other things that cords or ropes could be attached to. In an article published by the American Psychiatric Association, some psychiatrists worried the new rules could be too expensive or could result in psychiatric units closing.
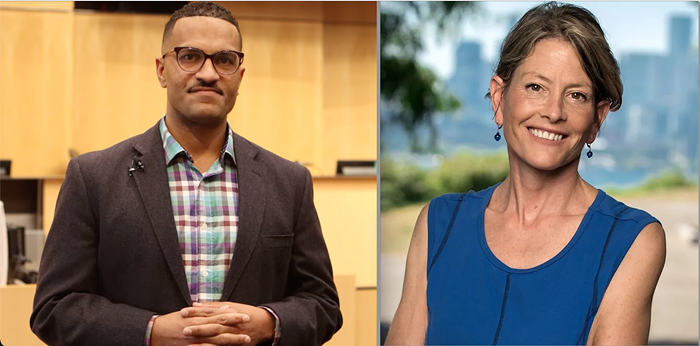
Staff at the UWMC psychiatric unit have heard rumors about the unit closure for months, but got the most recent update during a meeting Thursday with UWMC Executive Director Geoff Austin. According to minutes of the meeting taken by a staff member, Austin identified “significant” budgetary challenges, including the new ligature regulations. According to the minutes, one nurse raised concerns about Washington’s shortage of psychiatric beds and the potential that the closure could contribute to illegal boarding of patients. Another asked whether layoffs are in store and how they might happen. Cindy Sayre, Chief Nursing Officer for UW Medicine, responded, “As soon as I know we will deliver that message,” according to the minutes.
The Washington State Nurses Association, which represents a small number of nurses in the unit, said in a statement the potential closure is disappointing, “not only because of the potential loss of jobs for our union members” but also because of the “severe shortage of inpatient psychiatric beds in Washington State.”
Anxiety about the potential closure is extending beyond just the nurses who may lose their jobs. A clinician at Harborview who spoke on the condition of anonymity called the potential closure “a tragedy.” The clinician said they believe Haborview could absorb much of the demand that would have otherwise gone to UWMC if the unit closes. Harborview, which is also part of UW Medicine, already regularly has people waiting for its 65 to 70 beds.
“It’s not what the people of Washington need right now,” the clinician said. “I understand people look at black numbers and red numbers on a ledger sheet, but what are we here for? Are we here to turn a profit or are we here for the people of Washington State?”