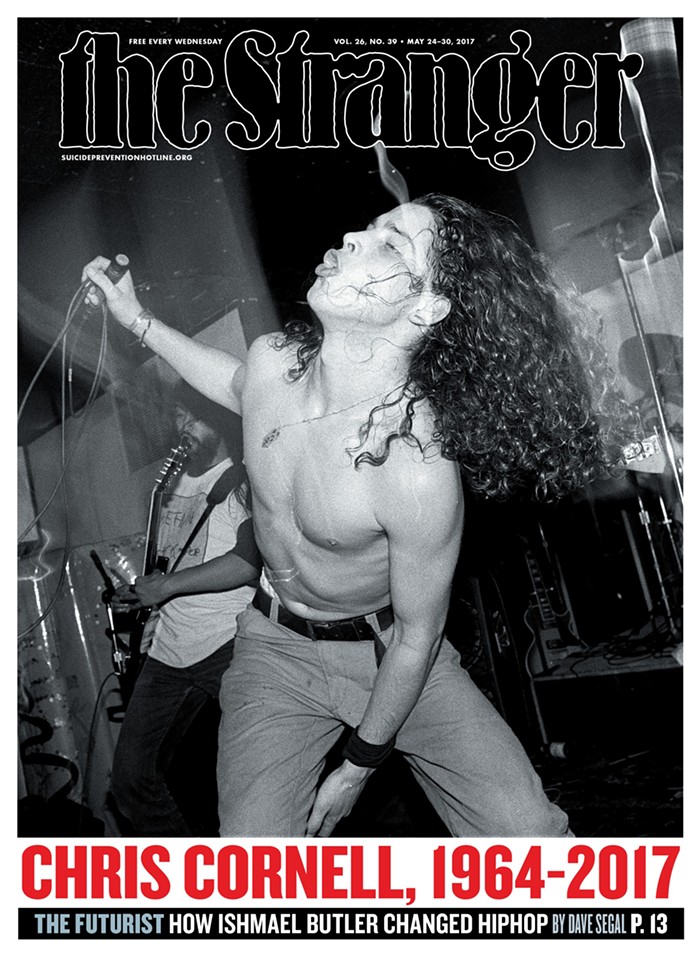
Jonathan Golob is the former science columnist for The Stranger and presently a professor of Infectious Diseases and Internal Medicine at the University of Michigan School of Medicine.
On Monday, March 16, he made national news as one of three experts in a lawsuit filed by the American Civil Liberties Union (ACLU) against the US Immigration and Customs Enforcement (ICE). According to Newsweek, the ACLU wants ICE "to release detainees who are believed to be at 'high risk' of facing serious health consequences if they contract COVID-19 in the event of an outbreak at the Tacoma Northwest Detention Center." Golob provided this legal action with a testimony.
He also appeared in a recent Engadget post, "Health experts explain how we should be cleaning our gadgets." He recommended that "If you touch something contaminated, such as your phone, after hand washing, you need to wash it again to clear the virus away."
On March 18, I had a conversation with Golob that explored three aspects of the present pandemic: one, that's historical; the second, pathological; and the third, social (or cultural). The historical aspect compared the present pandemic with the one between 1918 and 1919. That flu killed around 30 million people and had a mortality rate comparable to COVID-19, 2.5 percent. But unlike COVID-19, it hit hardest people in their physical prime (15 to 34-years-old).
Golob is not a medical historian, but he is certain of one thing: The influenza pandemic of 1918 was very deadly because evidence-based medical knowledge at the time was in its infancy. In the 100 years between now and then, a vast amount of knowledge concerning microbes and the behavior of infections in general was gathered. And this knowledge, if properly applied can make the present pandemic less lethal. But we live in an age where we are scientifically aware of many dangers but do next to nothing about them.

On the pandemic of 1918.
"In 1918, the germ theory was still a relatively new concept," Golob said. "There were people alive who grew up in the era of miasma," which was the belief that "diseases such as cholera, chlamydia infection, or the Black Death were caused by 'bad air.' This is not our situation. A century later, we know better. The pandemic is not ambiguous. [US] public health experts as early as January were ringing the alarm bells, as the reports came out of the human-to-human transmission in places like Wuhan. So, in 1918, there were questions about how best to even deal with a pandemic."
Plus, of course, you had World War I. "You had people in barracks and in training camps and in the trenches. You can't socially distance during war. And then you are in an era when you don't have antibiotics, you don't have ventilators and medicine as we know it today, evidence-based medicine, medicine that had finally moved beyond a millennia of bloodletting and all of that kind of crap. The [Influenza Pandemic of 1918] was an era when people were just beginning to learn how to actually effectively treat infections."

On the medical or pathological aspects of COVID-19.
"So, human beings are constantly exposed to coronaviruses of all manner all of the time. It's one of the most common causes of the regular old cold," Golob said.
"The thing that's unique about this is it is a novel infection. What that means is that the newness of the virus is the essence of the problem. It is different than what any person on Earth has experienced. Now, what we know is that COVID-19 has a good enough fit to spread from person to person, but it does not have a good enough fit to be relatively benign infection. This is the key point of the problem. If you think about evolutionary selection, there's a couple of solutions for a virus: one, being very virulent, which is not necessarily a bad solution for a virus. It can make people very sick very quickly to the point of death and all it has to worry about is being able to still spread from one person to the next in an effective way. But some of the most widespread infections don't take that path. Their impact can be so small that the infected person doesn't even know they are ill... Keep in mind that there's a whole collection of viral infections that many of us get as children, and if we are healthy for the most part, we really don't notice them though our lives.
"Now, with this novel coronavirus," he went on, "it's in this equipoise; it can kind of go either way—become mild or virulent. At this moment, it's relatively neither. Neither side is quite ready for each other. This is why one of the operating theories of this virus is focused on a person's reaction to it. It can be too extreme, and this can do more damage to one's health than the disease itself. So, one of the treatments that's being attempted, on an experimental basis right now, is to actually give people a very specific kind of immunity suppression, when they start getting very sick from the infection, with the idea that you have to tamp down the overreaction to this new, this novel thing."

On the importance of progressive social (cultural) policies during the present pandemic.
"The most salient point I can see out of all of this is that South Korea and other places, like Taiwan, and Singapore, really leaned into the era, and used all of the available tools, all of the advanced molecular diagnostics and systems and logistics, and they used them for the general good, used them in a way that really, I think, bent the curve [of the infection rate]. Yes, people got sick, people died. I don't want to be too rosy about this. But really, truly, it was remarkable and inspiring. But we in the US don't hear about countries like South Korea or Singapore."
Why were they so effective?
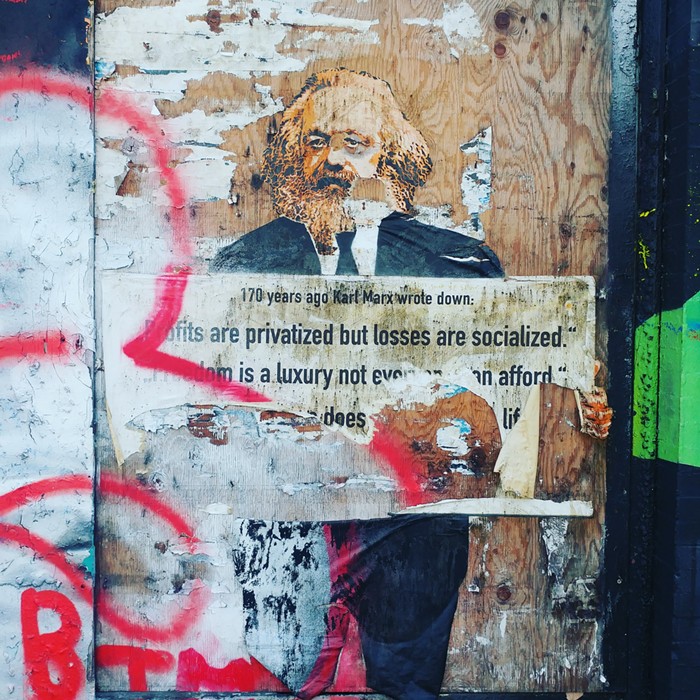
"Part of the reason why they were so effective might be cultural for two reasons. One, they had a memory of SARS. It happened around 2002. They saw and learned from the failures in their systems. So, they were prepared for the next big one. But these countries are also either social democratic, as in South Korean and Taiwan, or authoritarian socialist, as in Singapore. What this shows is that political systems with strong socialist or democratic policies will fare better in a pandemic than those that do not. The US is not one of those countries."
But Golob believes that if there's any place in the US that's "on track to have a softer blow from COVID-19, it's Seattle... Seattle has had the most cases and so on, but that's really because the city engaged early with the crisis. But when you compare Seattle to, say, a place in West Virginia, Seattle is far ahead. It made the appropriate measures, like physical distancing and closures and taking it seriously, finding the cases, identifying them, doing contact tracing. It's also important that Seattle is city with a $15 minimum wage and other progressive policies. These are going to help further soften the blow because in a crisis like this, you're only as safe as the most marginal people in your community."