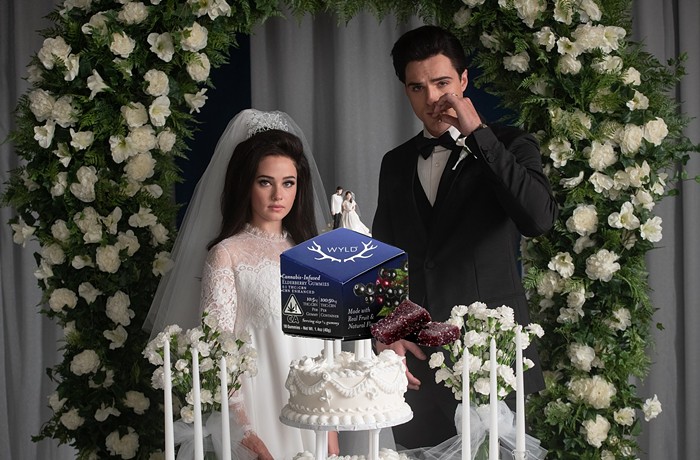
As a mysterious respiratory illness sweeps across the planet, medical marijuana patients and recreational users alike have been looking at their bongs and wondering: Is this a bad idea? In a wide-ranging interview about what he has seen at his clinic and in local hospitals, what he thinks of our state's response to the crisis, and what he believes personally about the benefits of cannabis, Dr. Sunil Aggarwal points out that not all delivery systems are the same. "Tinctures, edibles, non-smoke delivery methods, topicals—these are probably the safest" right now, the doctor says.
You went to medical school at the University of Washington. What has it been like for you living in the epicenter of the first COVID-19 outbreak in the US?
Well, initially we had such little to go on, and so everyone was really just playing things by ear, and nobody really knew. We still don't have a great sense of the contagiousness. So it was very frightening, nerve-racking, really, to know what advice to give our patients but also protect ourselves.
And what have you noticed over the last few weeks, since those first deaths?
I think over time we've really seen a lot of our community come together. We're marshaling the resources of infectious disease and virology departments at the University of Washington. And also one of the first vaccine trials is now happening at Kaiser Permanente Research Institute here in Seattle. And the guidelines the UW has been sending out every day and sharing with the larger community have really helped the community and the larger health care community feel like we've got a handle on this. And the governor and the state government have been proactive. I'm hopeful that these kinds of thing can happen for other major health crises that are always going on in this state, like homelessness and lack of access to basic health care—that's my hope.
When you say we still don't know about the contagiousness of COVID-19, what do you mean exactly?
Well, you know, there were a lot of questions about droplet spread, whether you need droplet protections or aerosolized protections, how much contact protections, all these different aspects are a little unknown. There was that well-reported case of people coming down with COVID even though they were practicing six-feet separation when they had choir practice up in Skagit County, in Anacortes. Several people died because of contacting COVID likely during that choir practice. So forceful breathing is suspected as one of the mechanisms to get this more broadly airborne beyond droplets.
Your clinic integrates cannabis into patients’ wellness plans. Have you changed what you tell patients about cannabis in light of COVID-19?
Already medicinal cannabis use is not a shared activity. This is really about minimizing contact with other peoples' germs. The question of whether cannabis itself will suppress or lower the immune threshold that makes you more susceptible—we have no evidence of that. The International Association on Cannabinoid Medicines put out a statement at the end of last month that there's no evidence that cannabis could be used to treat COVID-19, but there's also no evidence that it could increase the risk of viral infection. They also acknowledge there are clinical studies that show that cannabinoids could have anti-viral, anti-bacterial effects. So it has not really come up at my clinic, in any major way. My naturopathic medicine colleagues are really experts at thinking about how to help support people's immune functions, to keep them at their best level of health. The American Association of Naturopathic Physicians has recommended intravenous vitamin C be given to patients—that they should be given to patients in hospitals who are effectively sick with COVID...
Intravenous vitamin C?
Yeah, yeah. It's based on good data that's come out of China. But there's other things happening—there's so much. It's not my specialty, but I'd certainly pay attention to the folks who are working on patient support from a naturopathic or holistic perspective. I'm also hoping that patients in the hospital will get the plasma...
The plasma?
The most exciting thing I'm hearing about is the plasma, where you get plasma from people who've survived COVID, so you can build up your immune response and help fight it.

It has been reported that tobacco smokers are at greater risk of death from this coronavirus than non-smokers. Do you know if there is any data about cannabis smokers and COVID-19?
I haven't seen anything. But certainly we know that smoking with cannabis, regularly heavy users can have more chronic bronchial irritation, and may be more susceptible to bronchitis. The term is called "pulmonary toilet"—like, how effective is your bronchial system at clearing and getting rid of mucus, viruses, bacteria, debris? There might be a little less sturdy function in people who have chronic exposure to smoke. But there's no relationship to cannabis smoking and development or COPD or lung cancer. That's been definitively found in large studies—
Wait, really?
Yes. Yes, Dr. Tashkin at UCLA has shown that nicely. It's mentioned in a couple epidemiological studies. And then also there's been some nice data lung function in a study called the CARDIA study that was done published out of UCSF. It was a multi-center large study that studied peoples' lung function for years, and actually, people who used cannabis had a little bit improved pulmonary dynamics. Like, ability to blow air faster. Some of those dynamics were improved in cannabis users in a large study that was published a number of years ago. But that may not help you in fighting COVID-19. But it could be a question if your bronchial irritation might impair pulmonary toilet. In general, doing everything we can to improve your lung function with a virus that causes severe acute respiratory distress syndrome is important.
I'm still wrapping my head around the phrase "pulmonary toilet."
[Laughs.] Yeah, I'm sure your readers will enjoy that.
So you do acknowledge that smoking cannabis might be a bad idea right now considering this is a respiratory illness?
In general, smoke, anything that irritates your lungs, in general, if you can minimize that with non-smoke delivery, that's probably better for your lungs. What's the threshold where it causes excessive irritation or inflammation? It's going to vary from person to person. And it's also the dose and the degree. But I can say there's a relationship between regular cannabis use and bronchial irritation.
If I smoke a bong regularly, after six months or a year I notice tar builds up in it at every joint all throughout the device—is that tar also going into my lungs?
You know, you are getting exposed to soot. But the difference between your device and your body is your body is alive and has all sorts of internal cleaning systems, so it processes things. They don't just hang out there, these particles. They get processed. As long as your system is healthy, you're able to clear things.
And are tobacco smoke and cannabis smoke different in terms of how they affect you?
There's some data that said that some of the toxins called polycyclic aromatic hydrocarbons (PAHs) that are made as combustion byproducts, or things like benzopyrene that are also found in tobacco smoke—those chemicals get cleared from the lungs after smoke exposure gets into the bloodstream. But then it has to get through a conversion process in the liver where it gets turned into a more carcinogenic compound, but it turns out the enzymes that do that are inhibited by cannabinoids. So there could be some pharmacological protective actions of the cannabinoids in protecting against some of the impacts of the smoke on the body's health. There's a whole article called "Cannabis and Tobacco Smoke Are Not Equally Carcinogenic" that was published in the Harm Reduction Journal ten or fifteen years ago by Dr. Robert Milimede. These are not simple questions. It's very complicated. But in general, if your system gets overwhelmed, and your pulmonary toilet is not functioning, you can get some irritation.
You're blowing my mind with cannabis smoke not being linked to COPD or lung cancer. That's amazing.
The National Institute on Drug Abuse will say that: "Oh, it's still an open question." But I don't think it is. There's a party line and there's the quality data that's out there. I've written that and published that in peer-reviewed journals, and many others have too.
How do you view vaping? We heard all these health scares about vaping in the fall.
Oh yeah, all that vaping scare had to do with what we already knew for a long time: that certain solvents should not be used in those devices. Propylene glycol, vitamin E acetate—these things we shouldn't be adding to something that is low heat that's then being brought to our lung system. The original vaping was dry-flower vaping: low-heat, low-combustion on flower. And then of course concentrates took off, and that's really where this Wild West thing took off. But people who don't use solvents? We don't have any evidence that you're putting anything into your body except cannabis resin at low heat.
Although vaping can still make you cough.
There still can be some irritation of the lungs with vaping, so patients and consumers have to know to try not to get themselves too thick of an exposure. The vapor cloud shouldn't be as thick. You can find ways to, like, inhale air and mix in with the vapor, so it's not as concentrated, because that can be irritating to the respiratory tree, and cause coughing and irritation.

Is it a bad idea to share pipes, bongs, and other devices that you touch to your mouth?
Well yeah. At this time, it would go against the six-feet-away precautions. But I guess in families, people who are staying home are probably sharing things, so that's probably fine. Continue as normal, as long as people aren't sick. But I think at this time, we never really know who might be a carrier, so it's probably safer to avoid. Or if you're going to share things, sterilize them.
But you are not recommending to anyone to completely stop using cannabis, even recreational users.
Recreation to me is really an aspect of the spiritual use of cannabis—spiritual health and well-being. Because cannabis helps people find meaning and joy and bliss, and that's so important to health, so I don't want to minimize that. And I think also this whole idea of sharing things, you know, finding some way to connect—it's vital for our health too. So I think we should find ways to maintain that, but safely, so we don't put each other at risk.
If someone is going to consume cannabis right now, what's the safest way to do it?
Tinctures, edibles, non-smoke delivery methods, topicals—these are probably the safest in that regard. As long as you have good, clean products.
What are the medical conditions for which cannabis is most effective?
Chronic pain, muscle spasms, nausea, vomiting, loss of appetite. Those are probably the top ones.
You are also an expert in palliative care and end-of-life issues. What do you make of all these COVID deaths happening in isolation? Have you seen anything like this before?
No. It's so difficult. Difficult for the patient, feeling like they're dying without their loved ones present, which is such a critical need. Universally, people ask for their loved ones present at the end of life. And then of course it's difficult for the families not to have presence with their loved ones for the grieving process. These situations are just so hard. I know our community is working so hard to try to use video and virtual and telephone, and that I think can help to substitute at this time. You know, people also aren't even able to have birthing attendants, either, at the other end [of the cycle of life]. I've heard of hospitals not allowing that for women in labor.
This is brutal, what we're living through.
We're having to come into life and leave life under conditions of a pandemic. And we can just do the best we can. The health workers are sometimes able to be present—nurses are doing that. And they're also helping facilitate connection through virtual. At one of the hospitals I work in, they are allowing for people who are at the end of life, who aren't COVID-positive, they're allowing them to have some more visitors. They're lifting some of the visitor restrictions. Like, they can have two visitors rather than just one in the whole course of the day. So it's impacting people across the whole board, not just COVID deaths, but deaths in medical health care facilities or nursing homes, from everything.
I guess it makes sense to loosen restrictions on someone who's at the end of life anyway, because what's the worst that can happen?
We still have to make sure that those people who come in are screened, they don't have fevers, and there should be universal masking in all the health facilities. But the need for the patient to have a good death, and for the family not to be traumatized by not being there, is a consideration. And that lets the hospital administration know, like: "Okay, for these folks, visitors can come a little bit more liberally, because they're never going to see their loved one alive again."
Are you personally wearing masks when you go grocery shopping? Should people be wearing masks to the pot store?
Yes, at this point, I am wearing a mask when I leave the house now. The CDC has recommended masking when you go outdoors, mostly to protect other people from you. But yes, any time you're out in public, wearing something in the pot shop or anywhere is smart and might reduce your exposure and definitely will reduce your droplets on other people, so it's good.
You are the co-founder and co-director of the AIMS Institute, which stands for Advanced Integrative Medical Science. Are you still able to see patients in this time of stay-at-home?
Yes. We are doing telemedicine. We've been set up to do telemedicine from our very beginning. Thankfully insurance companies including Medicare have lifted all their restrictions on that, and just recently the state has mandated that they have to pay us the same amount—the insurance companies have to pay us equal, have to reimburse us at the same rate for virtual visits. So some of those barriers are being lifted thanks to the actions of the government in this crisis. There are still some things we're still doing in person that just have to be done. We just practice lots of precautions. We're an essential business, but we're doing what we can from a distance.
Speaking of this phrase "essential business." What is your reaction to the rather abrupt about-face from some government entities who not long ago considered cannabis distribution as a crime and now consider it an essential part of society?
[Laughs.] Yeah. Just, uh... [Laughs.] A smile and a laugh. That's my response right now. Things are changing. The other day I got to speak about cannabis to some of the leaders of the National Institutes of Health, the National Cancer Institute, the National Institute on Drug Abuse (NIDA)—a bunch of these NIH institutes, especially NIDA, that have really avoided and ignored this entire beneficial framework. So the fact that I could talk to them for 40 minutes at a national public thing was a shift. That hadn't happened. Of course, these things are going to definitely impact how we perceive the role of cannabis in society after we get past this pandemic.
Do you perceive a world in which we see all sorts of things, including cannabis and medicine, differently, after we've moved through this crisis?
I certainly do feel that that's a possibility. So many major disasters lead to big changes in society afterwards, for the better, because we kind of figure out what our priorities are. That's actually the nature of serious illness, too. When people get sick, sometimes there's an opportunity to be better than you were before you got sick. And so I hope that happens writ large for society.